Show summary Hide summary
- How menstrual pads became silent fertility trackers
- From lab strip to smart menstrual cycle monitoring
- What fertility changes these smart pads can actually show
- Where menstrual pad diagnostics meet apps and wearables
- From home bathroom to population-level research
- Can a menstrual pad really measure my fertility?
- How accurate is hormone detection in menstrual blood compared with a blood test?
- Will these pads replace my period-tracking app or wearable?
- Are there privacy concerns with smart menstrual pads and fertility tracking?
- Who might benefit most from pad-based cycle monitoring?
Every month, millions of women quietly discard something that may hold a detailed record of their future fertility. What if menstrual pads could turn that hidden information into real-time, at-home fertility tracking data, as easily as reading a pregnancy test?
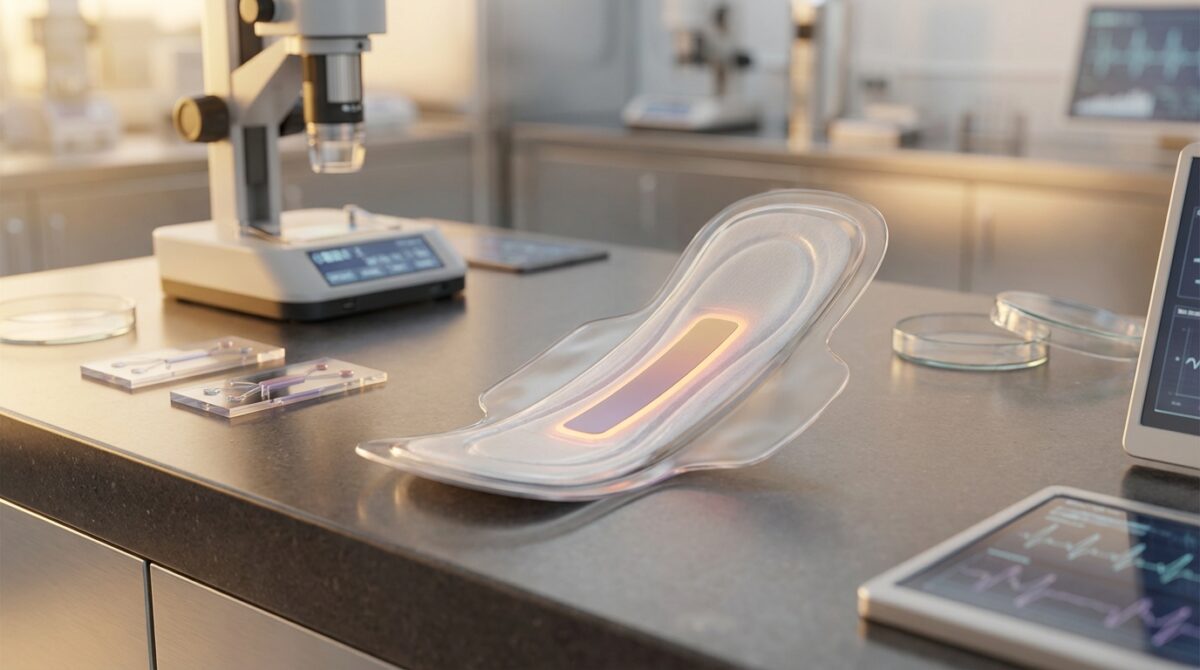
Researchers in Switzerland and health-tech innovators worldwide are now transforming period blood into a new kind of diagnostic signal. By embedding smart strips inside menstrual pads, they aim to turn routine cycles into a continuous window on ovarian health, hormone balance and long-term reproductive health.
How menstrual pads became silent fertility trackers
The turning point came when a team at ETH Zurich, led by Lucas Dosnon, asked a simple question: could the same biological markers doctors search for in blood be reliably detected in menstrual flow? Their focus landed on anti-Müllerian hormone (AMH), widely used in clinics as a proxy for “ovarian reserve”.
How Alzheimer’s Might Deceive the Brain into Self-Erasing Its Memories
Blurry Rats and Mange-Ridden Coyotes: Exploring the Quirky Subreddit Devoted to Identifying Mysterious Wildlife
AMH levels generally decline with age. Higher levels suggest a larger pool of remaining eggs, while unusually low values may hint at early menopause or reduced egg supply. Traditionally, women needed a venous blood draw or finger-prick kit sent to a laboratory. According to work reported alongside other smart pad concepts such as pads that turn period blood into data diagnostics, this new device pulls the lab into the pad itself.

The lateral-flow strip hidden inside the pad
The ETH Zurich group engineered a lateral flow assay, similar in concept to a COVID-19 rapid test. Tiny gold-coated particles are coated with antibodies that specifically bind AMH. When exposed to menstrual blood, they migrate along a strip embedded in the pad and form a visible line.
The darker this line, the higher the hormone concentration. Early validation work showed that AMH values measured from menstrual blood closely aligned with those obtained from standard laboratory serum tests, as also highlighted in coverage of a fertility insights pad prototype. That agreement suggests period blood can serve as a reliable matrix for hormone detection, rather than a messy by-product to be thrown away.
From lab strip to smart menstrual cycle monitoring
To move beyond a simple yes-or-no readout, the team trained a smartphone app to analyse photographs of the test line. The app converts colour intensity into an estimated AMH value, turning the pad into a connected medical device without adding bulky electronics.
This approach mirrors a broader wave of cycle monitoring technology. A narrative review in the American Journal of Obstetrics and Gynecology mapped more than twenty consumer tools for ovulation tracking and conception support, including devices discussed in research on fertility wearables and home devices. Yet most still rely on temperature curves, cervical mucus logging or urinary hormones rather than menstrual blood itself.
Why menstrual blood is a powerful biomarker source
Menstrual fluid contains blood, endometrial cells, immune molecules and circulating hormones. That makes it a rich source of biomarkers that reflect not only fertility but broader aspects of women’s health. Projects reported by ETH Zurich and others echo findings from teams who demonstrated that new pad devices can track signs of disease in period blood.
Researchers now view menstrual blood as a non-invasive sampling channel that repeats every month without needles or appointments. For someone like Sara, a hypothetical 32-year-old planning to delay pregnancy, regular AMH data from pads could reveal whether her ovarian reserve is stable, slowly declining or unexpectedly low for her age.
What fertility changes these smart pads can actually show
AMH cannot predict exactly when menopause will occur or guarantee the success of in vitro fertilisation. Specialists such as Richard Anderson from the University of Edinburgh caution that no test can directly measure egg quality. Still, tracking relative fertility changes over years may help women ask better questions, earlier.
High AMH levels may point towards conditions like polycystic ovary syndrome, while extremely elevated values can, in rare circumstances, be linked to granulosa cell tumours of the ovary. Continuous monitoring through pads could prompt timely clinical follow-up instead of waiting until pregnancy difficulties arise. Articles on how periods may help flag disease risk underline this potential.
Beyond AMH: towards multi-hormone fertility tracking
Smart-pad innovation is not limited to ovarian reserve. At consumer-tech showcases, companies such as Vivoo have presented FlowPad, a concept pad that quantifies follicle-stimulating hormone (FSH) to support perimenopause and fertility tracking. Coverage of this product in reports on FlowPad hormone tests illustrates how FSH levels can map shifts in the late reproductive years.
Alongside this, Qvin’s Q-Pad, described in features on pad-based lab tests, collects menstrual blood for laboratory analysis, including PAP-smear-like screening. These efforts all point towards pads as quiet, recurring biosensors woven into everyday life rather than special-purpose devices stored in a drawer.
Where menstrual pad diagnostics meet apps and wearables
Smart pads are emerging alongside a mature ecosystem of apps and wearables for menstrual cycle analysis. Research reviewed in studies on hormonal health and period-tracking apps shows how digital tools have shifted from pure fertility prediction to holistic wellness dashboards.
Advanced algorithms now combine heart rate variability, sleep patterns and temperature, as seen in frameworks such as machine-learning based ovulation prediction models. Integrating pad-derived hormone readouts into these systems could vastly improve cycle monitoring accuracy, especially for people with irregular periods.
From home bathroom to population-level research
For clinicians and public health scientists, anonymised data from thousands of pad tests could reveal how ovarian reserve patterns vary across regions, pollution levels or socioeconomic groups. Publications like innovative approaches to menstruation and fertility tracking highlight how citizen-generated data can reshape research on reproductive health.
This has implications beyond individual family planning. Longitudinal hormone patterns may intersect with environmental exposures, nutrition and stress, areas already explored by sustainability-focused organisations such as initiatives linking health and environment. In that sense, menstrual blood becomes not only a personal health indicator but also a probe of how modern lifestyles affect biology over decades.
- Early signal of ovarian decline: repeated AMH measurements can show whether values are dropping faster than expected for age.
- Insight into endocrine disorders: unusually high or fluctuating levels may prompt evaluation for PCOS or other hormone imbalances.
- Support for IVF timing: clinicians may use long-term trends to refine when to consider assisted reproduction.
- Broader disease screening: as shown in research on disease-detecting pads, period blood can carry markers of cancer or inflammatory conditions.
- Education and autonomy: regular feedback can help users understand their own cycles and advocate for tailored care.
Can a menstrual pad really measure my fertility?
Smart pads do not measure fertility in an absolute sense, but they can estimate levels of hormones such as anti-Müllerian hormone or FSH in menstrual blood. Those values provide indirect information about ovarian reserve or perimenopausal status, especially when tracked across multiple cycles and interpreted with medical guidance.
How accurate is hormone detection in menstrual blood compared with a blood test?
Early validation studies suggest that AMH values derived from menstrual blood align closely with conventional serum measurements. The lateral-flow strips and smartphone analysis are calibrated against laboratory assays. However, clinical decisions still rely on professional evaluation, and these devices are positioned as complementary tools rather than full replacements.
Will these pads replace my period-tracking app or wearable?
Smart pads are more likely to expand the information available to your existing tracking tools rather than displace them. Apps and wearables already capture timing, temperature and heart rate changes. Integrating pad-based hormone readings would add biochemical context, creating a richer picture of ovulation timing, cycle variability and long-term reproductive trends.
Are there privacy concerns with smart menstrual pads and fertility tracking?
Groundbreaking DNA Study Recasts the History of the Beachy Head Woman
Unlocking the Power of Our Microbiome: The Century’s Most Groundbreaking Insights
Any system that digitises health data raises legitimate privacy questions. Responsible providers should offer transparent data policies, local processing when possible and options to opt out of data sharing. Users are encouraged to read privacy statements carefully and choose solutions that align with their expectations for confidentiality and data security.
Who might benefit most from pad-based cycle monitoring?
Women considering delaying pregnancy, those undergoing fertility treatment, or people with irregular or painful cycles may find particular value in recurring hormone insights. Smart pads can also support research in under-served populations where access to clinics and laboratory testing remains limited, bringing more equitable monitoring options into everyday life.